Address
Road no. 4, Vatara, Notun Bazar
Dhaka, Bangladesh
Address
Road no. 4, Vatara, Notun Bazar
Dhaka, Bangladesh

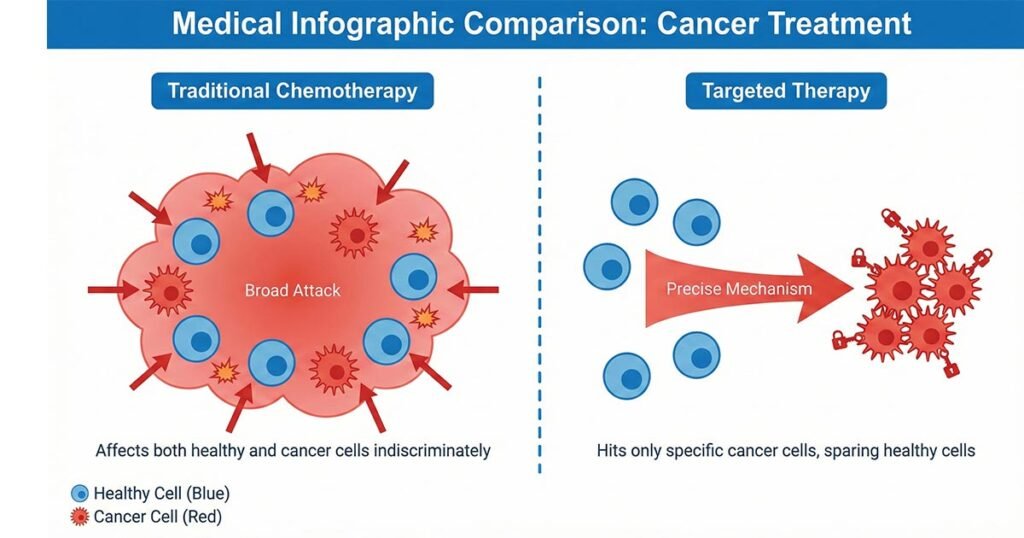
For decades, the word “blood cancer treatments” brought a single image to mind: chemotherapy. While effective, traditional chemotherapy is known for being a “carpet bomber”—it attacks all fast-growing cells in the body, which includes cancer cells but also healthy cells in your hair follicles, stomach lining, and bone marrow. This is why treatment has historically been so difficult on the body.
However, the landscape of blood cancer care—specifically for Leukemia and Lymphoma—has undergone a revolution. We have entered the era of Targeted Therapy.
Unlike chemotherapy, targeted therapies are “snipers.” They are sophisticated medications designed to identify and attack specific genetic mutations or proteins that cancer cells need to survive, often leaving healthy cells unharmed. For many patients, this means fewer severe side effects and the convenience of taking a daily pill at home rather than spending hours attached to an IV drip in a hospital.
In this guide, we will walk you through how these modern treatments work for different types of blood cancer (like AML, CLL, and CML), how to manage common complications like low platelet counts, and how generic oncology medications are making these life-saving treatments accessible and affordable for everyone.
Acute Myeloid Leukemia (AML) is an aggressive cancer that starts in the bone marrow. In the past, treatment options were limited. Today, doctors first test your DNA to see if your cancer has specific “mutations” (errors in the code) that are driving the growth. If you have one of these mutations, there is likely a pill designed specifically to shut it down.
Some patients with AML have a mutation in the IDH1 or IDH2 genes. These genes normally help cells produce energy. When mutated, they produce a harmful substance that stops young blood cells from maturing into healthy adults. Instead, these immature cells pile up and become cancerous.
Patient Tip: These drugs can sometimes cause a condition called “differentiation syndrome,” where the blood cells mature too fast and cause inflammation. If you experience fever or shortness of breath, contact your doctor immediately—it is treatable!
The FLT3 mutation is one of the most common mutations in AML. Think of FLT3 as a switch that is stuck in the “ON” position, constantly telling cancer cells to multiply.
In a healthy body, old or damaged cells are programmed to self-destruct—a process called apoptosis. Cancer cells, however, are clever. They overproduce a protein called BCL-2 that acts like a shield, protecting them from dying.
Chronic Lymphocytic Leukemia (CLL) and Mantle Cell Lymphoma (MCL) are cancers of the B-cells (a type of white blood cell that fights infection). A key player in the growth of these cancer cells is a protein called Bruton’s Tyrosine Kinase (BTK).
BTK is part of a signaling pathway that tells B-cells to stay alive and divide. BTK inhibitors are drugs that sever this communication line.
Ibrutinib was the first drug in this class and changed the game for CLL patients. It is a daily pill that has allowed many patients to live for years without chemotherapy. However, because it was the first, it sometimes affects other proteins off-target, which can lead to side effects like heart rhythm issues. If you have been prescribed Ibrutinib, [Ibruxen] is a high-quality generic alternative available.
Science never stops improving. Acalabrutinib is a “second-generation” inhibitor. It was designed to be more selective, hitting the BTK protein with greater precision while ignoring other healthy proteins. This often results in fewer side effects (like less bleeding or heart risk) compared to Ibrutinib, making it a preferred choice for many new patients. You can find this advanced therapy listed as [Acaluxen].
CML is treated with drugs called Tyrosine Kinase Inhibitors (TKIs). Most patients do well on standard TKIs (like Imatinib), but sometimes the cancer mutates again and becomes resistant. The most difficult mutation to treat is called T315I.
Treating the cancer is only half the battle. Both the cancer itself and the treatments can destroy your platelets—the tiny cells responsible for clotting blood. When platelets get too low (a condition called Thrombocytopenia), you are at risk of dangerous internal bleeding or bruising.
To treat this, doctors use TPO Receptor Agonists. These are not cancer drugs; they are “boosters” that tell your bone marrow to wake up and produce more platelets.
Eltrombopag is a widely used oral medication for raising platelet counts in patients with ITP (Immune Thrombocytopenia) or those with Hepatitis C.
Avatrombopag is a newer option that is becoming very popular because it is more convenient. unlike Eltrombopag, it does not have dietary restrictions, meaning you can take it with food without worrying about calcium interference. It is often used for patients with chronic liver disease who need a surgery or procedure. For a modern, patient-friendly option, see [Avalet].
A common question patients have when browsing online is: “Is it safe to buy generic cancer medication?”
The answer is a resounding yes, and understanding why can save you thousands of dollars.
When a pharmaceutical company invents a new drug (like Ibrutinib or Venetoclax), they get a patent that allows them to be the only seller for a few years. This is why brand-name drugs in the US or Europe can cost $10,000 or more per month.
However, once that patent expires (or in countries where patent laws differ), other certified manufacturers can produce the exact same medication.
Generic drugs are required to be “Bioequivalent.” This means:

The only differences are usually the inactive ingredients (like the binding paste that holds the pill together), the color of the pill, and—most importantly—the price.
Because generic manufacturers didn’t have to spend billions on research and advertising, they can sell the drug for a fraction of the cost. At Onus Pharma, we specialize in sourcing these high-quality generics to ensure that financial barriers never stop you from getting the treatment you deserve.
A blood cancer diagnosis is overwhelming, but the options for treatment have never been better. Whether you need a precise FLT3 inhibitor like [Gilternib], a BCL-2 blocker like [Ventoxen], or supportive care with [Avalet], modern medicine allows for targeted, effective treatment plans.
By choosing generic options, you are not compromising on quality; you are simply choosing to make your care sustainable.
Disclaimer: This content is for educational purposes only and does not constitute medical advice. Always consult your oncologist before starting or changing any medication.