Address
Road no. 4, Vatara, Notun Bazar
Dhaka, Bangladesh
Address
Road no. 4, Vatara, Notun Bazar
Dhaka, Bangladesh
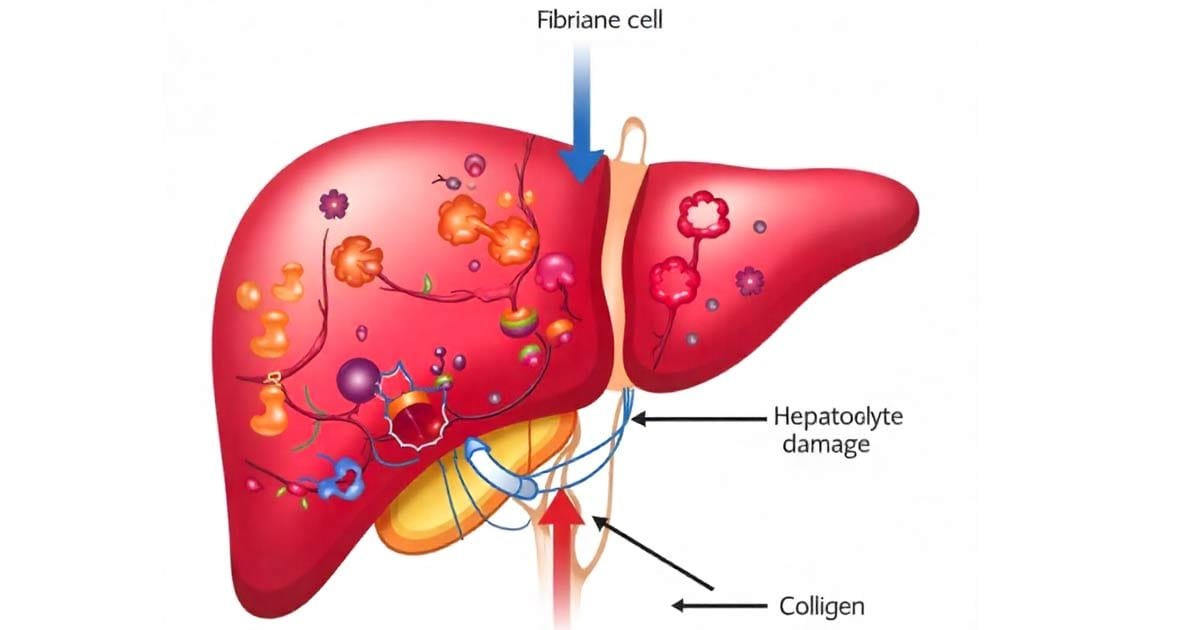
Fibrosis is the formation of large amounts of abnormal scar tissue in the liver, which is called liver fibrosis. It means, when the liver tries to recover the damaged cells after being damaged repeatedly for a long time, and damage continues, scar tissues are produced instead of healthy liver cells, and when they are formed in large amounts in the liver, it turns into liver cirrhosis.
The liver repairs itself by making new and healthy liver cells after every injury, even if it is severe, and attaches them to the web of connective tissue in replacement of dead liver cells.
If scar tissues are produced, they perform no function like liver cells do; instead, they interfere with blood flow and limits the blood supply for the liver cells. Without enough blood flow, the number of healthy cells dies more than previously and forms more scar tissue in the liver. When it happens, blood pressure is increased in the vein that carries blood from the intestine to the liver, which is also known as portal hypertension.
Liver fibrosis can be caused by liver disorders, medication, and substances that damage the liver.
Metabolically–dysfunction–associated steatosis occurs in people with excessive body weight, diabetes or prediabetes, and high levels of fats and cholesterol in the blood. This combination of risk factors for fatty liver disease is also known as metabolic syndrome. In the last few years, metabolic syndrome has become increasingly common. Additionally, Viral hepatitis B is also a common cause of liver fibrosis, and sometimes the reason is unknown.
Liver fibrosis has no pain or other symptoms, even if it is in the advanced stage or has become cirrhosis. Though there are some symptoms you can be alert for severe fibrosis or cirrhosis, listed below
Doctors suspect fibrosis if the patients have a liver disorder or are taking medication that can cause fibrosis. Then they perform liver tests, including blood tests, imaging tests, and a liver biopsy. If they find any traces of fibrosis or a damaged or malfunctioning liver, they perform other tests to determine the stage of the fibrosis and its severity.
Imaging tests are performed through ultrasonography, (CT scan) computed tomography scan, and (MRI) magnetic resonance imaging. In this process, early or moderately advanced fibrosis detection is not possible. It can only show the abnormalities that can accompany cirrhosis and portal hypertension.
Certain combinations of blood tests can differentiate between absent or mild fibrosis and moderate to severe fibrosis. The detection of the severity of fibrosis helps indicate the prognosis in people who have chronic viral hepatitis.
Liver biopsy is another reliable way to detect the stage of fibrosis and identify the disorder that causes fibrosis. A biopsy is performed to identify the cause of the liver disease, the stage level of the fibrosis, or the presence of cirrhosis, as well as the response rate to the treatment. Before performing a liver biopsy, doctors will do blood tests and imaging tests to determine the level of fibrosis, as a biopsy is invasive and can cause complications.
Specialized Imaging tests are used to detect the stiffness of the liver tissue, where the more stiff the liver tissue, the severe liver fibrosis is likely to be. Specialized imaging tests like transient elastography, magnetic resonance elastography (MRI), and acoustic radiation force impulse imaging use sound waves that are applied to the abdomen to determine how stiff the liver tissue is.
Transient elastography and magnetic resonance elastography are being used to diagnose liver fibrosis in patients and to stage the fibrosis. Additionally, as conventional ultrasonography results rely on the skills of the person, these tests are also performed to check the amount of fat in the liver in fatty liver disease.
A combination of the blood tests and specialized imaging tests may improve the doctor’s ability to accurately assess the degree of the fibrosis.
Sometimes fibrosis can be reversed if the main reason is identified and treated properly. Fibrosis becomes widespread and permanent after continual and repeated damage to the liver cells. The scar tissue can destroy the liver’s internal structure, impairing the liver’s ability to reproduce liver cells and function.
Focusing on treating the cause often slows down the further scarring of the liver and results in improvement. These treatments include
Ways to reduce your risk of developing fibrosis may include:
References:
https://www.merckmanuals.com/home/liver-and-gallbladder-disorders/fibrosis-and-cirrhosis-of-the-liver/fibrosis-of-the-liver (by Tae Hon lee-MD, Icahn School of Medicine at Mount Sinai)
https://www.hoag.org/specialties-services/digestive-health/diseases-conditions/liver-fibrosis/?
https://www.radiologyinfo.org/en/info/fatty-liver-disease
Disclaimer: This information is provided for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your doctor or another qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read here.